Understanding HIPAA violations: Types, prevention, and best practices

The Health Insurance Portability and Accountability Act (HIPAA) is a crucial framework designed to protect patient privacy and ensure the security of personal health information (PHI). Its importance cannot be overstated, as compliance safeguards sensitive data and enhances the trust between healthcare providers and patients.
The complexity of healthcare operations can often lead to lapses in compliance, highlighting the necessity for ongoing education and vigilance among staff. HIPAA violations not only jeopardize patient trust but can also lead to extensive investigations by regulatory bodies, resulting in further scrutiny and potential operational changes.
This blog aims to educate readers about HIPAA violations, their implications, and effective strategies for prevention.
What Is a HIPAA Violation?
Understanding HIPAA violations is critical for maintaining the integrity of patient care. HIPAA violations occur when there is a failure to comply with the regulations set forth in the act, resulting in unauthorized access, use, or disclosure of protected health information.
Violations can arise from both intentional actions, such as data breaches, and unintentional mistakes, like mishandling patient information.
Compliance with HIPAA is essential for healthcare organizations to avoid legal repercussions, financial penalties, and damage to their reputation. It also fosters respect for patient privacy and trust in the healthcare system.
Also read: HIPAA-covered entities
Protected Health Information (PHI)
PHI includes any individually identifiable health information that is held or transmitted by a covered entity, such as:

Common types of HIPAA violations
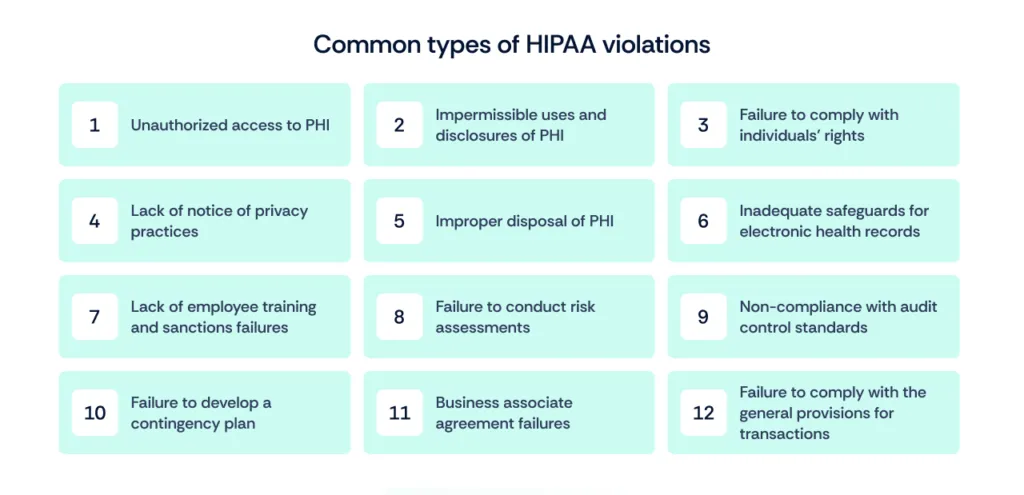
Understanding the common types of HIPAA violations is essential for healthcare organizations to safeguard patient privacy and ensure compliance with federal regulations.
1. Unauthorized access to PHI
This violation happens when individuals access patient information without proper authorization, potentially leading to breaches of confidentiality.
2. Impermissible uses and disclosures of PHI
Impermissible uses and disclosures occur when patient health information is accessed or shared without appropriate consent or authorization. This can lead to severe penalties and a loss of trust from patients.

3. Failure to comply with individuals’ rights
Patients have specific rights regarding their Protected Health Information (PHI), including the right to access their records and request corrections. Failure to uphold these rights can result in compliance violations.
4. Lack of notice of privacy practices
Healthcare organizations are required to provide a Notice of Privacy Practices that informs patients how their PHI is used and their rights under HIPAA. Failing to provide this notice can lead to violations.
5. Improper disposal of PHI
When healthcare organizations do not dispose of PHI securely, they risk exposing sensitive information to unauthorized individuals.
6. Inadequate safeguards for electronic health records
Failing to implement adequate security measures for electronic health records can expose sensitive patient data to cyber threats.
Organizations must implement appropriate physical and technical safeguards to protect PHI from unauthorized access. A lack of these safeguards can expose sensitive information to breaches.

7. Lack of employee training and sanctions failures
Insufficient training for employees regarding HIPAA regulations can lead to inadvertent violations and mishandling of patient information. Additionally, failing to implement sanctions for non-compliance can lead to repeated violations.
8. Failure to conduct risk assessments
Not regularly conducting risk assessments leaves organizations vulnerable to potential threats and non-compliance issues, making it harder to protect PHI effectively.
9. Non-compliance with audit control standards
HIPAA requires organizations to implement audit controls to monitor access to PHI and detect potential security violations. Non-compliance with these standards can result in undetected breaches.
10. Failure to develop a contingency plan
Organizations must have contingency plans in place to address data breaches or emergencies affecting PHI. A lack of such plans can lead to inadequate responses in critical situations.
11. Business associate agreement failures
Covered entities must have Business Associate Agreements (BAAs) in place with third parties that handle PHI on their behalf. Failing to secure these agreements can lead to significant compliance issues.
12. Failure to comply with the general provisions for transactions
HIPAA sets standards for electronic transactions related to healthcare. Non-compliance with these provisions can result in administrative penalties and hinder efficient healthcare operations.
Also read: How to map HIPAA to ISO 27001
Consequences of HIPAA violations
The penalty for HIPAA violations range from financial penalties, legal repercussions, and damage to reputation.
A. Financial penalties
Healthcare organizations found in violation of HIPAA can face substantial financial penalties. The penalty for HIPAA violation can range from thousands to millions of dollars depending on the severity and nature of the violation. These fines can significantly impact the financial health of an organization, diverting funds away from patient care and services.
What is the maximum penalty for violating HIPAA? The maximum penalty for HIPAA violation can reach up to $2,067,813 per year for each violation category, depending on the severity and intent of the breach.

B. Legal repercussions
In addition to financial penalties, HIPAA violations can lead to legal actions, including lawsuits from affected patients. Organizations may also face investigations from the Office for Civil Rights (OCR), which can result in further legal consequences and increased scrutiny.
HIPAA violations can lead to imprisonment, particularly in cases of willful neglect or malicious intent. The law stipulates that individuals found guilty of knowingly violating HIPAA can face criminal penalties, including fines up to $250,000 and imprisonment for up to 10 years, depending on the severity of the violation.
C. Damage to reputation and trust
A HIPAA violation can severely damage an organization’s reputation, leading to a loss of patient trust. Patients are less likely to share sensitive information with providers that have a history of non-compliance, which can ultimately impact patient care and organizational success.
Also read: Who enforces HIPAA?
Strategies to avoid HIPAA violations
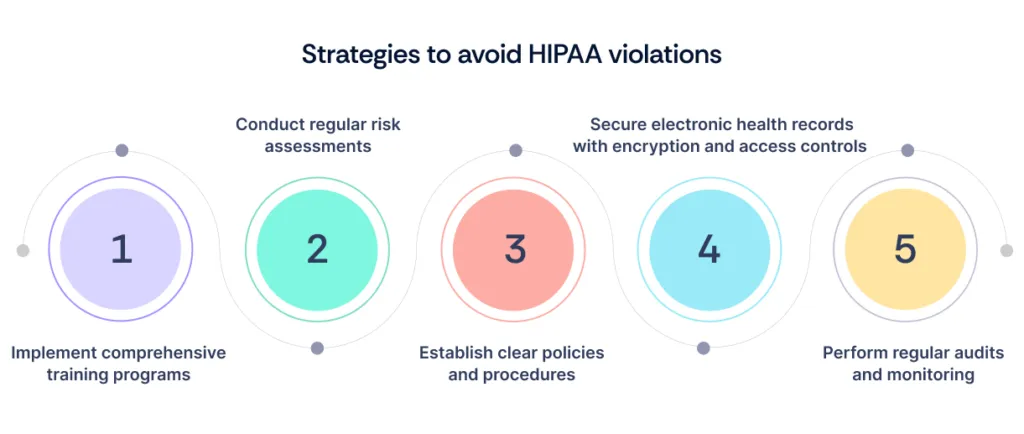
Here are the top strategies to avoid HIPAA violations and any related penalty for HIPAA violations.
A. Implement comprehensive training programs
Regular training programs for all employees are crucial to ensure everyone understands HIPAA regulations and the importance of protecting patient information. This should include ongoing education to keep staff updated on best practices.
Scrut offers tailored training modules that educate employees on HIPAA regulations and best practices, ensuring they remain compliant and knowledgeable about patient information protection.
B. Conduct regular risk assessments
Regular risk assessments help identify potential vulnerabilities within an organization’s systems and processes. By proactively addressing these risks, organizations can better protect PHI and ensure compliance.
With Scrut’s automated risk assessment tools, organizations can easily identify vulnerabilities in their systems and processes, allowing for timely remediation and enhanced protection of PHI.
C. Establish clear policies and procedures
Developing and enforcing clear policies and procedures related to PHI handling, access, and security is essential. These guidelines should be communicated effectively to all employees to ensure consistent adherence.
Scrut facilitates the development and communication of clear policies and procedures regarding PHI handling, ensuring that all employees are aware of their responsibilities and can adhere consistently.
D. Secure electronic health records with encryption and access controls
Implementing robust security measures, such as encryption and strict access controls, can significantly reduce the risk of unauthorized access to electronic health records. These technical safeguards are essential for protecting sensitive patient information.
Scrut provides advanced security features to safeguard electronic health records against unauthorized access and breaches.
E. Perform regular audits and monitoring
Conducting regular audits and continuous monitoring of systems and practices can help detect potential violations early. This proactive approach allows organizations to address issues before they escalate into serious compliance problems.
Scrut’s continuous monitoring and audit capabilities enable organizations to detect compliance issues early, allowing for swift corrective actions before they develop into significant violations.
Also read: HIPAA compliance checklist
How to respond to suspected violations?

HIPAA violations must be reported to the Department of Health and Human Services (HHS) within 60 days of discovering the breach.
Failing to report within this timeframe can lead to increased penalties, including substantial fines and potential criminal charges, depending on the severity and nature of the violation.
Effectively responding to suspected HIPAA violations is crucial for maintaining security and compliance within your organization. Here’s how to go about it.
A. Report procedures within the organization
Establishing clear reporting procedures is essential for prompt action when a suspected HIPAA violation occurs.
Employees should be trained to recognize potential violations and understand the process for reporting them to designated compliance officers or an internal reporting hotline.
Ensuring confidentiality during the reporting process can encourage employees to come forward without fear of reprisal.
B. Investigate and address the issue
Once a suspected violation is reported, it is crucial to conduct a thorough investigation to determine the nature and scope of the issue.
This investigation should include:
- Gathering relevant information
- Interviewing involved parties
- Assessing the impact on protected health information
After identifying the cause, organizations must take corrective actions to prevent future occurrences and ensure compliance.
C. Notify affected individuals and authorities if necessary
If the investigation confirms a HIPAA violation that compromises patient data, organizations are required to notify affected individuals promptly.
Additionally, if the breach meets certain thresholds, it may also be necessary to report the incident to the OCR and other relevant authorities.
Timely notifications help maintain transparency and trust with patients while fulfilling legal obligations.
Also read: 13 best HIPAA compliance software
Wrapping up
Understanding and preventing HIPAA violations is essential for safeguarding patient privacy and ensuring compliance within healthcare organizations.
By prioritizing compliance and implementing effective strategies, organizations can mitigate risks and enhance their overall security posture.
Partner with Scrut to streamline your compliance efforts and strengthen your vulnerability management process—contact us today to learn how we can help!
Frequently Asked Questions
1. What are the most common types of HIPAA violations?
Common types of HIPAA violations include unauthorized access to patient information, failure to secure electronic health records, improper disposal of PHI, lack of employee training on privacy policies, and inadequate risk assessments.
2. What are the potential penalties for HIPAA violations?
Penalties for HIPAA violations can range from fines of $137 to $68,928 per violation, depending on the severity and nature of the violation.
3. How can organizations ensure HIPAA compliance?
Organizations can ensure HIPAA compliance by implementing comprehensive training programs, conducting regular risk assessments, establishing clear policies and procedures, securing electronic health records, and performing regular audits to monitor compliance.
4. What should I do if I suspect a HIPAA violation?
If you suspect a HIPAA violation, report it to your organization’s compliance officer or designated privacy official immediately. They will investigate the issue and take appropriate action, which may include notifying affected individuals and reporting the violation to the Department of Health and Human Services (HHS) if necessary.
5. Are there specific training requirements for staff to avoid HIPAA violations?
Yes, HIPAA requires organizations to train all employees on privacy and security policies. Training should cover handling of PHI, recognizing potential risks, and understanding the consequences of non-compliance. Regular refresher courses are also recommended to keep staff informed of any updates.
6. What is the civil penalty for unknowingly violating HIPAA?
The civil penalty for unknowingly violating HIPAA can range from $137 to $68,928 per violation, depending on the circumstances.